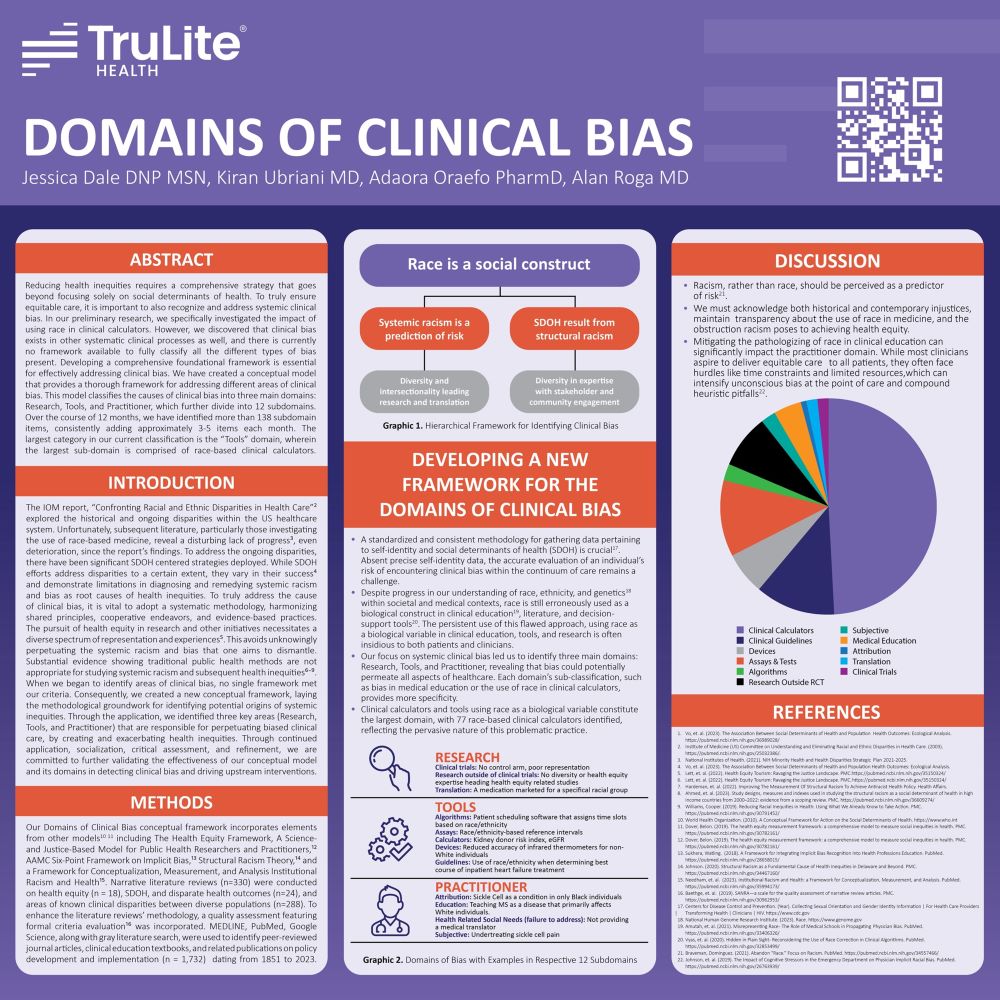
To truly close disparate care gaps and help all people receive equitable care, requires a strategy that doesn’t just focus on the traditional social determinants of health (SDoH), but one that boldly confronts the persistent issue of systemic clinical bias. To dismantle clinical bias, it’s essential that we endorse shared common principles, collaborative efforts, and scientifically grounded practices.
As a part of our work at TruLite Health, we’ve developed a novel conceptual framework to help identify potential sources of systemic inequities. Utilizing this framework, we’ve uncovered three significant domains – Research, Tools, and Practitioners – that contribute to bias in clinical care, consequently fueling health inequities. We remain steadfast in our commitment to apply, socialize, critically assess, and refine this conceptual model to further authenticate its effectiveness in identifying clinical bias and catalyzing proactive interventions.
Despite the scientific consensus that race is a social construct, the misuse of race as a biological construct persists in clinical education, literature, and decision-support tools. The continued use of race as a biological construct poses a risk to both patients and clinicians. It’s time we changed our perspective – racism, not race, should be identified as the risk factor. Recognizing historical and ongoing injustices, maintaining transparency about the role of race in medicine, and understanding the hindrance racism poses to achieving health optmization are key steps in our journey.
We will present our Clinical Bias Abstract at Mayo Clinic’s third annual RISE for Equity Conference.