Failure to deliver equitable care has significant downstream consequences, affecting the entire healthcare system. Biased care, even when unintentional, can lead to delayed diagnosis, advanced disease, and shorter life expectancy. An example of unintended consequences that can result from systemic disparities in guideline-recommended care. In 2017, JAMA completed a five-year study on surgical procedure volumes that helped shed light on the magnitude of these inequities, quantifying inequitable patient care.
In their January 2021 article titled, “Racial Disparities in the Use of Surgical Procedures in the US”, JAMA outlined disparities in the volume of surgical procedures on diverse populations. Even after adjustments for the US census division, hospital teaching status, or patient insurance status, these disparities persist. TruLite Health used the data presented in this article to summarize the impact experienced by Black individuals when compared to White individuals, for the most common procedures across coverage types. Regardless of the patient’s coverage type, there were a significantly lower number of procedures performed for Black individuals (graphic below).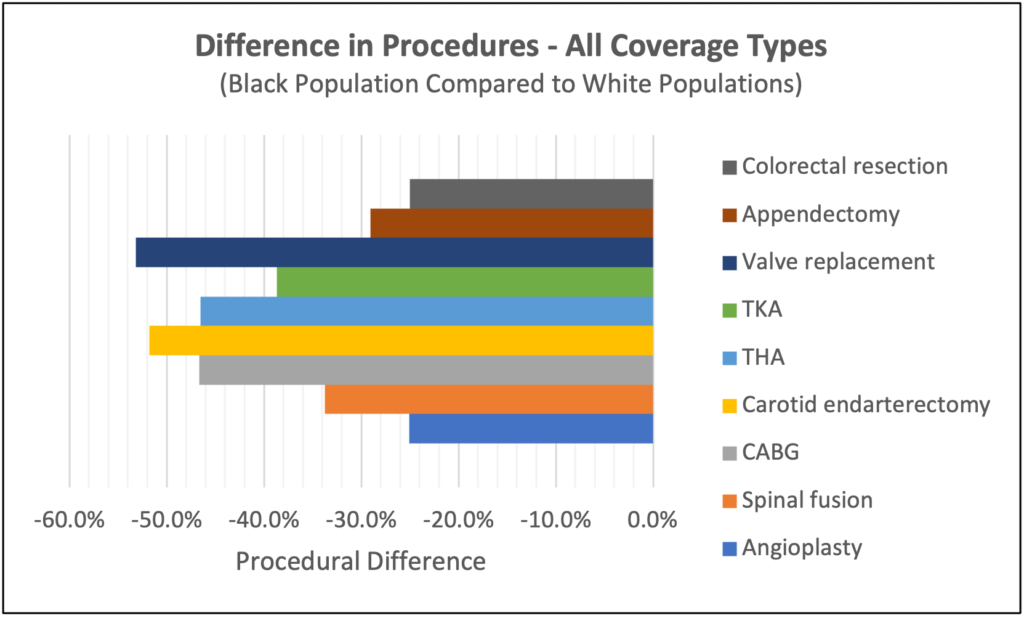 While individual situations may warrant that a procedure isn’t the best course of clinical care, performing 25% to 50% fewer procedures for a specific patient population indicates some form of bias along the care continuum. Numerous studies have demonstrated that Black individuals are considerably less likely to obtain guideline-concordant care, and this is true for conditions other than those depicted in the picture. Although this is only one facet of care delivery, the research shows that bias, including implicit and systemic, leads to disparities in care delivery.
While individual situations may warrant that a procedure isn’t the best course of clinical care, performing 25% to 50% fewer procedures for a specific patient population indicates some form of bias along the care continuum. Numerous studies have demonstrated that Black individuals are considerably less likely to obtain guideline-concordant care, and this is true for conditions other than those depicted in the picture. Although this is only one facet of care delivery, the research shows that bias, including implicit and systemic, leads to disparities in care delivery.
Examining differences in guideline-recommended procedure rates is a way that health systems and providers can work towards more equitable care for all. Learn more about how TruLite Health’s TruityTM platform can address health optmization at the point of care.